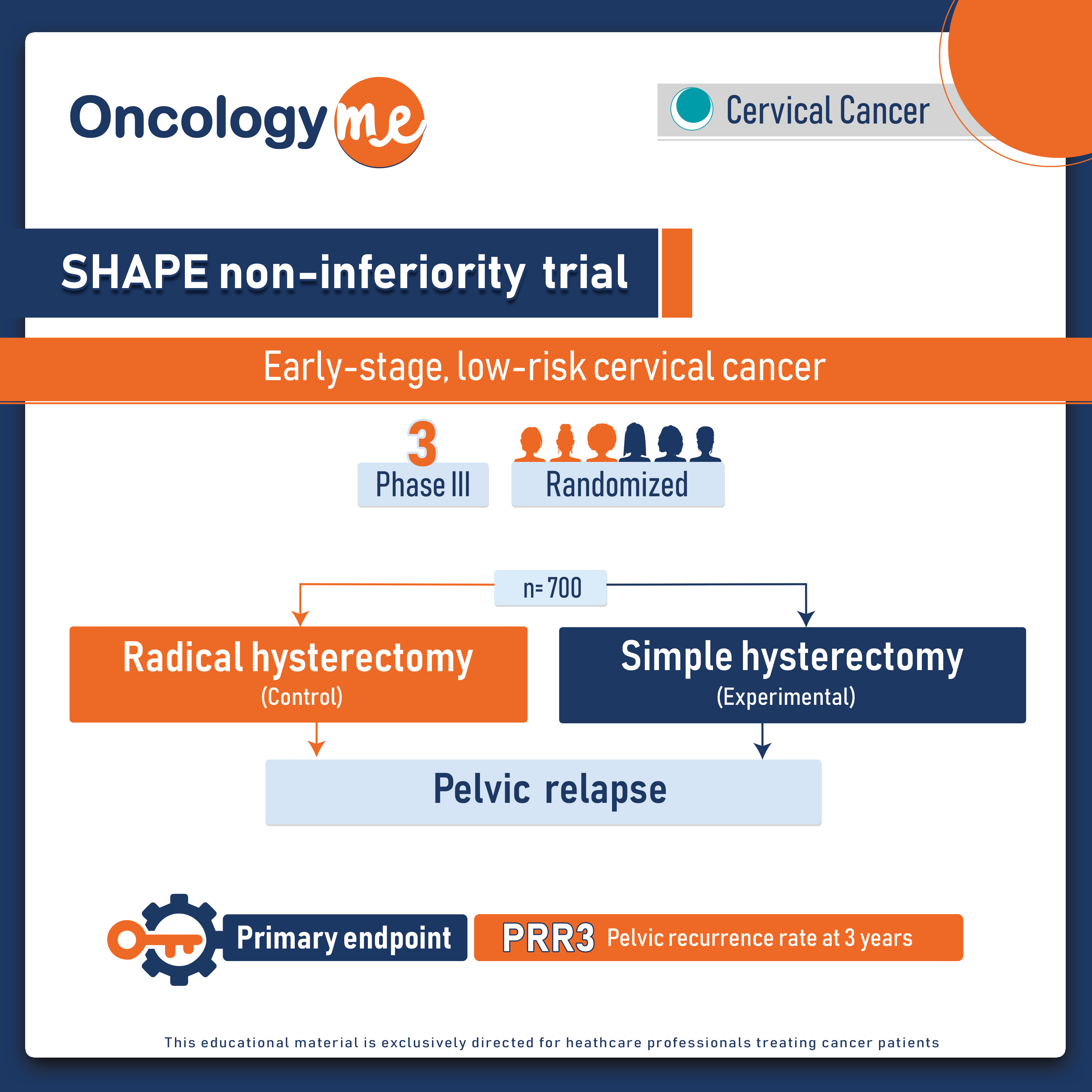
In the non-inferiority phase III prospective SHAPE trial, simple hysterectomy (SH) plus lymph node assessment was noninferior to radical hysterectomy (RH) plus lymph node assessment in carefully selected women with early-stage, low-risk cervical cancer. The 3-year rate of pelvic recurrence was 2.52% with simple hysterectomy compared with 2.17% with radical hysterectomy.
In this randomized trial, 700 patients with low risk early stage cervical cancer (LRESCC) defined as stage 1A2 or 1B1 with lesion ≤ 2cm , < 1 cm stromal invasion on preoperative LEEP or cone biopsy and < 50% stromal invasion on preoperative pelvic MRI. were randomized to RH or SH.
Patients were stratified by cooperative group, intended use of sentinel node mapping, stage, histological type, and tumour grade. The primary endpoint was pelvic recurrence rate at 3 years (PRR3).
Non-inferiority of SH to RH is claimed when the 95% upper one-sided confidence limit (95% UCL) for the difference in PRR3 of SH to RH (DPRR3), is lower than or equal to 4%. Primary intention to treat (ITT) analysis included all patients randomized. Per-protocol (PP) analysis included patients eligible at baseline and without evidence of more advanced disease found at the time of surgery or final pathology, based on treatment received. Secondary endpoints included extrapelvic relapse-free survival (ERFS), overall survival (OS), and quality of life (QoL).
Patient characteristics were well balanced: median age was 44 (24-80); 91.7% were stage 1B1 and 61.7% had squamous histology. 50% of the hysterectomies were done laparoscopically (56% SH vs. 44% RH), 25% robotically (24% vs. 25%) and 23% abdominally (17% vs. 29%). 4.4% of patients had lymph node metastasis (4.1% SH and 5.1% RH) and 3.1% had extrauterine extension (2.6% SH and 3.7% RH). A total of 8.8% of women received post-surgical adjuvant therapy (9.2% SH and 8.4% RH).
With a median follow-up of 4.5 years, 21 pelvic recurrences were identified (11 with SH and 10 with RH). The PRR3 was 2.5% with SH and 2.2% with RH (DPRR3 0.35% with 95% UCL 2.32% which didn’t cross the prespecified boundary of 4%) in ITT analysis; 2.8% with SH and 2.3% with RH (DPRR3 0.42% with 95% UCL 2.56% which also didn’t cross the prespecified boundary of 4%) in PP analysis. The 3-year ERFS and OS were respectively 98.1% and 99.1% with SH; 99.7% and 99.4% with RH. Meanwhile, Postoperative complications were more evident with RH compared to SH. RH had significantly higher rates of urinary incontinence (11.0% vs. 4.7% with SH; p=0.003) and urinary retention (9.9% vs. 0.6% with SH; p<0.0001) during follow-up. QoL scales with significant difference between the two groups over time were all in favor of SH.
This trial demonstrates the significance of well-planned studies in surgical oncology. The SHAPE study reveals that reducing the intensity of surgery can reduce the risk of complications without compromising the effectiveness of treatment for women with low-risk cervical cancer. "
.png)