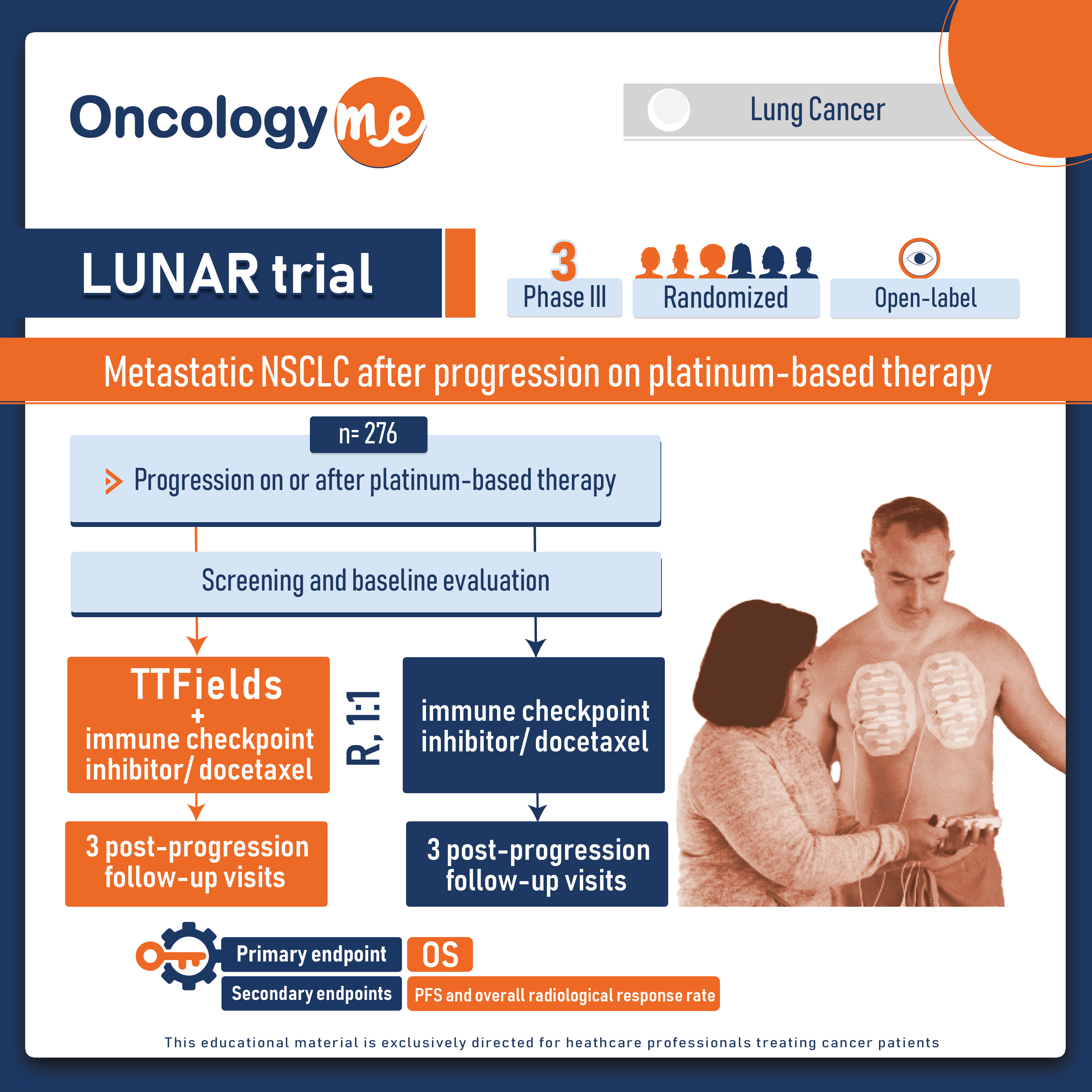
In the randomised, open-label, pivotal phase III LUNAR trial recently published in the LANCET Oncology, Tumor Treating Fields (TTFields) therapy added to standard therapy significantly improved overall survival compared with standard therapy alone in metastatic #NSCLC after progression on platinum-based therapy without exacerbating systemic toxicities.
In this randomized, multicenter trial, a total of 276 patients diagnosed with metastatic NSCLC, with either squamous or non-squamous histology, and who had experienced disease progression after platinum-based therapy, were enrolled. The study allowed for any number or type of previous lines of systemic therapy. The participants were randomly assigned in a 1:1 ratio to receive either TTFields therapy in addition to standard systemic therapy (investigator's choice of immune checkpoint inhibitor [nivolumab, pembrolizumab, or atezolizumab] or docetaxel) or standard therapy alone.
The TTFields therapy, delivered at a frequency of 150 kHz, was administered continuously to the thoracic region using a portable, at-home medical device. The therapeutic effect was achieved by applying 2 pairs of arrays to the chest, and it was recommended that patients strive for a minimum average device usage of 18 hours per day. To minimize potential skin irritation, the arrays were replaced every 3-4 days, with a slight shift in position of approximately 2 cm from the original placement.
Following disease progression, patients were offered salvage therapy at the discretion of the investigator. If patients discontinued the study systemic therapy due to disease progression outside of the field (while maintaining disease control within the field) or experienced intolerable toxicity from the systemic therapy, they were still eligible to receive TTFields therapy alongside the next line of salvage therapy.
The primary objective of this trial was to assess overall survival in the intention-to-treat population.
The combination of TTFields therapy and standard therapy demonstrated significantly improved overall survival compared to standard therapy alone (median 13.2 ms vs 9.9 ms; HR=0.74, p=0.035). In the subgroup of patients treated with immune checkpoint inhibitors, the addition of TTFields therapy also resulted in significantly improved overall survival compared to immune checkpoint inhibitors alone (median 18.5 ms vs 10.8 ms; HR=0.63, p=0.030). However, in the subgroup receiving docetaxel, there was no significant difference in median overall survival between TTFields therapy plus docetaxel and docetaxel alone (median 11·1 ms vs 8·7 ms, HR=0.81, p=0.28).
In terms of safety, serious adverse events were reported in 53% of patients receiving TTFields therapy plus standard therapy and 38% of patients receiving standard therapy alone in the safety population of 267 patients. The most frequent grade 3-4 adverse events included leukopenia (14%), pneumonia (10%), and anemia (8%). 71% of patients experienced TTFields therapy-related adverse events, which were mainly grade 1-2 skin and subcutaneous tissue disorders (85%).
TTFields therapy has the potential to revolutionize the treatment landscape by significantly improving survival rates in patients with metastatic NSCLC who have progressed on platinum-based chemotherapy. This innovative treatment approach addresses an urgent unmet need in this patient population, offering a promising alternative for enhanced therapeutic outcomes.
.png)