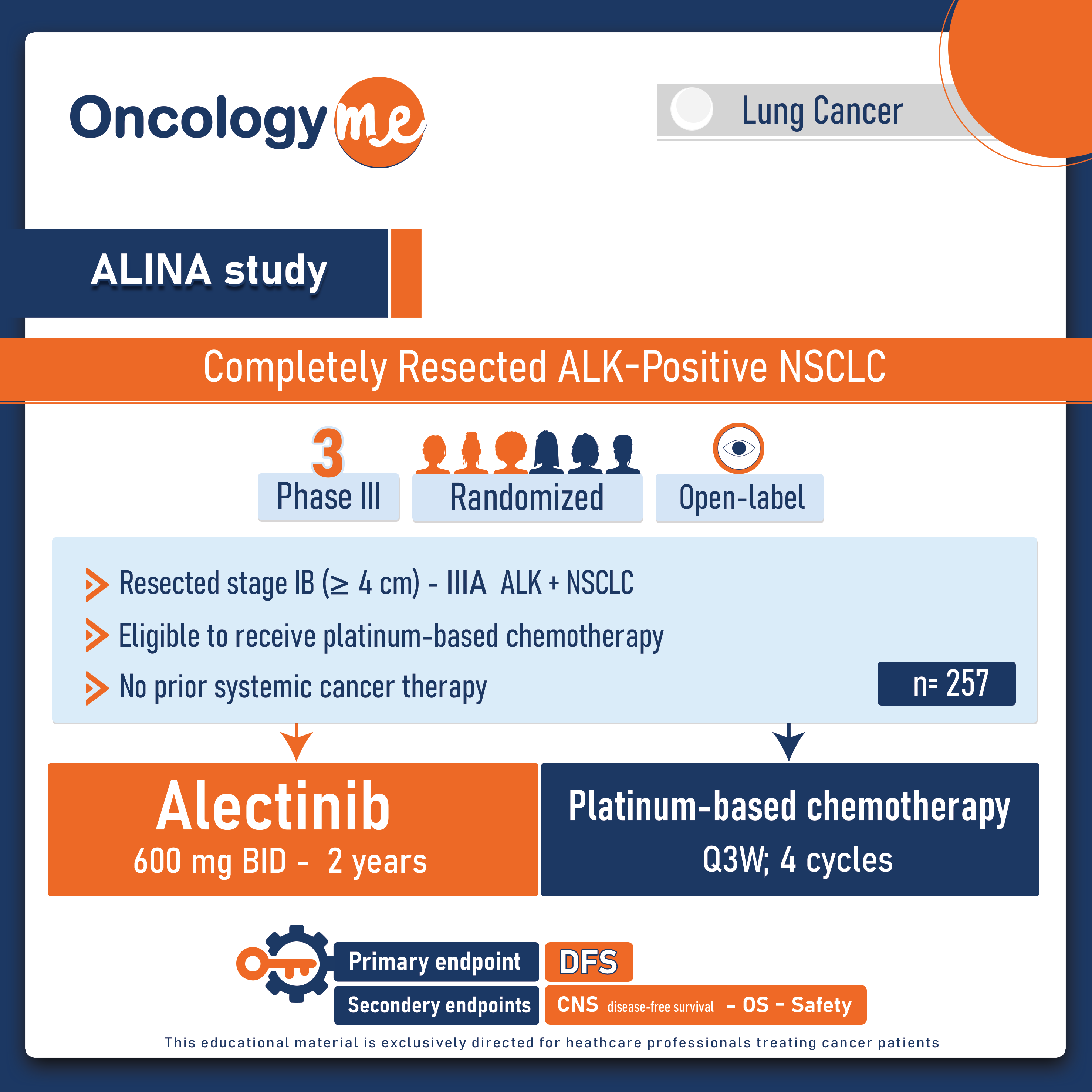
Practice-changing findings from a next-generation #ALK inhibitor were presented for patients with completely resected ALK-positive non-small cell lung cancer (#NSCLC) by Dr. Ben Solomon at the ESMO2023. In the prespecified interim analysis of ALINA, a global, phase III, open-label, randomised trial, #Alectinib proved to be the first ALK inhibitor to significantly improve DFS compared with CT in patients with completely resected ALK+ NSCLC.
In this practice changing trial, 257 eligible patients with completely resected, stage IB (≥4 cm)–IIIA, ALK+ NSCLC (per UICC/AJCC 7th edition) were randomised 1:1 to receive either oral alectinib 600 mg twice daily, or up to four of IV platinum-based CT q3w. Alectinib was given for a total period of 24 months or until disease recurrence, unacceptable toxicity. The Primary endpoint was disease-free survival (DFS), tested hierarchically first in the stage II–IIIA and then in the ITT population (stage IB–IIIA). Other endpoints included: CNS-DFS, overall survival (OS), safety.
After median follow up of 27.8 months, Alectinib demonstrated statistically significant and clinically meaningful improvement in the DFS compared to CT in both the stage II–IIIA (HR 0.24; p<0.0001) and ITT populations (HR 0.24; p<0.0001). This translates to a remarkable 76% reduction in the risk of recurrence or death. the median DFS was not reached for alectinib vs 41.3 months for chemotherapy. At 36-months, DFS rates were 88.3% vs 53.3% in the stage II–IIIA and 88.7% vs 54% in the ITT populations. The DFS benefit was consistent across all subgroups. Importantly, a clinically meaningful CNS-DFS benefit was observed in the ITT population as well (HR 0.22; 95% CI 0.08–0.58). The OS data are still immature.
The safety and tolerability profile of alectinib align with previous findings in studies of alectinib in the metastatic setting. Grade 3–4 adverse events (AEs) were reported in 30% of patients receiving alectinib and 31% receiving chemotherapy. There were no grade 5 AEs in either treatment arm. Overall, 13% of patients receiving alectinib had serious AEs compared with 8% receiving chemotherapy, but the rates of serious treatment-related AEs and AEs leading to treatment withdrawal were lower with alectinib (2% and 5%, respectively) compared with chemotherapy (7% and 13%, respectively).
These groundbreaking findings provide strong support for the use of alectinib as the standard of care in the early stages of lung cancer with ALK+ mutations. Given the scarcity of effective treatment alternatives available at present, the potential of alectinib to fill this therapeutic void becomes even more significant.
.png)