In the recent update of phase II PHERGain study, a #PET-based, pCR-adapted, chemotherapy free HER2 dual blockade strategy was associated with a substantial 3-year iDFS in patients with stage I-IIIA, #HER2+ early #breast cancer (EBC). These results appear comparable to those reported in several studies for the combination of neoadjuvant CT and dual HER2 blockade.
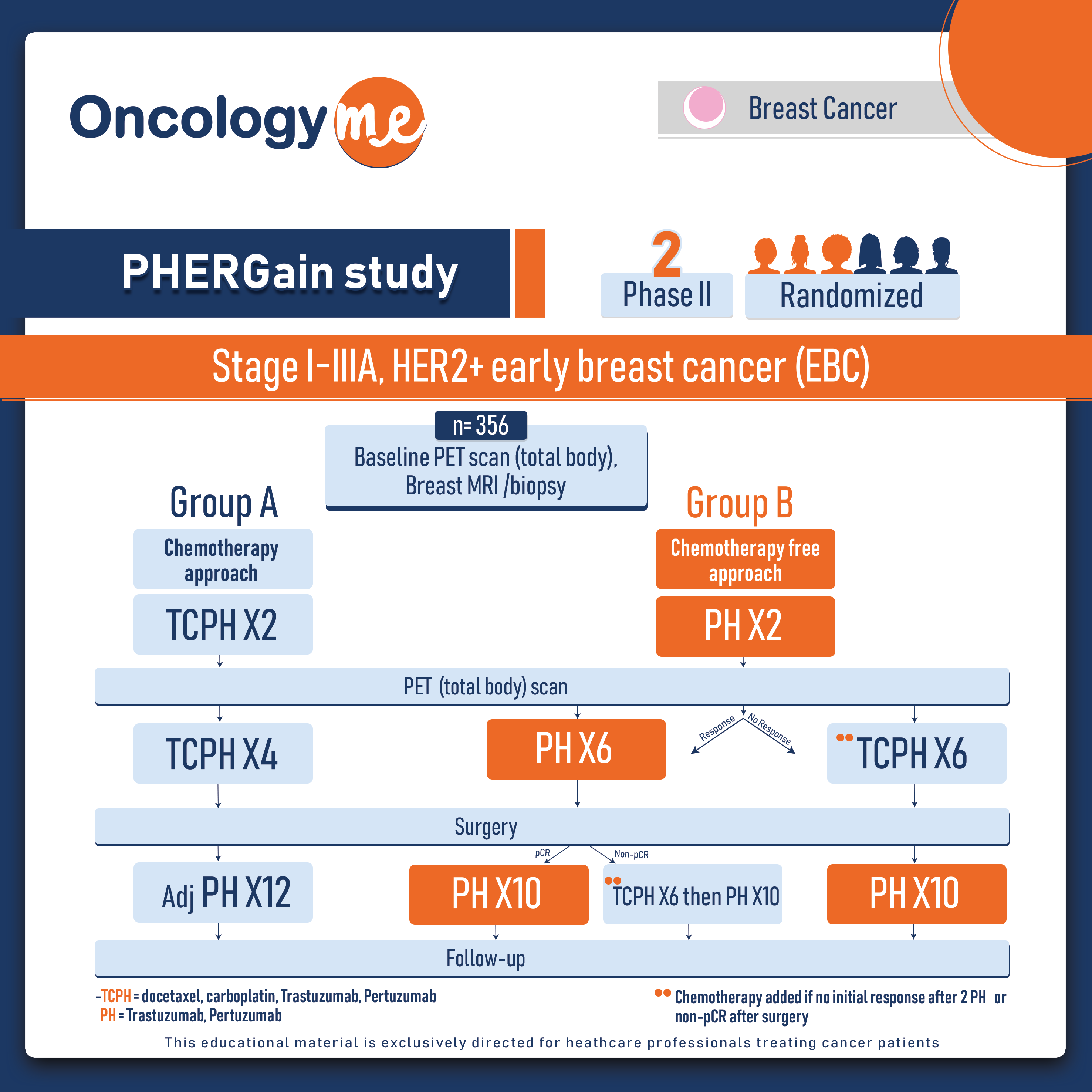
This noncomparative randomized study included 356 patients with stage I-IIIA, HER2+ disease and whose tumors were at least 1.5 cm. Approximately half the patients had N+ disease, about two-thirds had HR+ disease. patients were randomly assigned to one of the following groups: Group A received HER2 blockade with trastuzumab and pertuzumab plus chemotherapy docetaxel and carboplatin (TCHP) for initial two cycles (n = 71) and Group B who received dual HER2 blockade alone with pertuzumab, trastuzumab (PH) for initial two cycles as well (n = 285).
After two cycles, patients underwent total-body F-18 FDG-PET scans. Patients were considered PET responders if the scan showed a reduction in breast lesions of at least 40% from baseline. Afterthat, patients in group A (TCPH) remained there regardless of their response for four more cycles of TCHP. While Responders in group B (PH) continued with dual HER2 blockade alone (PH) for 6 more cycles, Non-responders in group B (PH) were switched to the TCHP group for six more cycles.
Upon completion of the assigned treatment, patients underwent surgery and were assessed for pCR. Group A (TCHP) then switched over to receive adjuvant PH for 12 cycles. Meanwhile, In Group B (HER2 blockade alone), patients with pCR received 10 cycles of adjuvant PH, whereas those without a pCR switched over to adjuvant TCHP for six cycles plus PH for four cycles. Patients with HR positive disease in all arms also received adjuvant endocrine therapy.
The primary endpoints focused on group B: the HER2 blockade alone arm. The first was pCR in PET responders (ypT0/isN0), and the second was 3-year invasive disease free survival (IDFS) in that arm.
The study met its primary endpoint which were published in The Lancet Oncology. A total of 227 (79.7%) of 285 pts included in group B were PET-responder, of whom 37.9% (86 pts) achieved a pCR (p<0.0001), reaching the first primary endpoint. In the updated analysis for iDFS after a median follow-up of 43.3 months, the 3-year iDFS rate for the group B/PET-responder was 95.4%, meeting the second primary endpoint (p<0.001). Moreover, in group B/PET-responder with pCR, the 3-year iDFS rates was 98.8%.
Treatment-related adverse events (AEs) and serious adverse events (SAEs) were higher in pts allocated to group A than to group B (grade ≥3, 61.8% vs. 32.9% [p<0.001]; SAEs, 27.9% vs. 13.8% [p=0.01]). Group B/PET-Responder with pCR presented the lowest incidence of treatment-related grade ≥3 AEs (1.2%) without any SAEs. No treatment-related deaths were reported.
These encouraging findings create a basis for the cautious implementation of dual HER2 blockade with selective chemotherapy de-escalation. By utilizing this strategy, approximately one-third of early-stage breast cancer patients with HER2+ tumors can potentially forgo chemotherapy with noteworthy reduction in associated side effects.
.png)